Menopause introduces a whole new set of changes to a woman’s life. When we think of menopause, hot flashes, trouble sleeping, and mood swings are common topics — but pelvic floor health is often overlooked. Hormonal changes during this time can contribute to pelvic pain, incontinence, and discomfort during sex. The good news is there are plenty of things you can do to improve your pelvic floor health during and after menopause!
How Menopause Effects the Pelvic Floor
Menopause officially begins when you haven’t had a menstrual cycle for 12 consecutive months. Most women experience menopause between the ages of 45-55. Symptoms will usually start earlier during premenopause which is the years leading up the menopause where your hormone levels start to fluctuate. During this time, estrogen levels begin to drop.
Why Hormones Matter: Estrogen and Your Pelvic Floor
Estrogen is essential for maintaining the health and elasticity of the tissues in your pelvic floor, which support your bladder, bowel, and uterus. When estrogen levels drop during menopause, these tissues begin to weaken, leading to uncomfortable symptoms like vaginal dryness, pain during sex, and even pelvic organ prolapse.
As the vaginal walls and surrounding tissues become thinner, drier, and less elastic, you may experience discomfort during intercourse, mild bleeding, or a raw sensation. Additionally, these hormonal changes can decrease your libido and increase the risk of urinary infections, as the tissues in your vaginal and bladder areas become more prone to irritation and infection.
Symptoms of Pelvic Floor Dysfunction During Menopause
As your hormone levels change, you might notice some of these common symptoms of pelvic floor dysfunction:
- Urinary incontinence: Leaking when coughing, sneezing, or exercising.
- Vaginal dryness: Decreased lubrication due to lower estrogen levels.
- Pelvic pain or discomfort: Especially during sexual activity.
- Prolapse: A feeling of heaviness or bulging in your vagina.
- Decreased sexual desire: A common result of hormonal shifts.
- Frequent urination or urgency: Needing to urinate often or urgently, even at night.
- Vaginal atrophy: vaginal walls may lose some of their natural stretch and lubrication, causing the vagina may shorten and narrow.
- Wind or faecal incontinence: Weakening of the pelvic floor muscles due to hormone changes may lead to difficulty controlling gas or bowel movements.
These symptoms can be challenging, but there are several ways to manage and even prevent them.
Managing Pelvic Pain and Intimacy During Menopause
Menopause can make sex feel uncomfortable or even painful, but that doesn’t mean you can’t continue to have a fulfilling sex life. Many women find that with the right adjustments, they can still enjoy intimacy well into their later years.
Here are a few strategies to help ease discomfort:
- Moisturise: Use natural moisturisers such as Olive & Bee Intimate Cream and Yes Vaginal Moisturiser Gel to keep your vaginal tissues hydrated. Apply these around the vaginal opening, your labia and inside your vagina regularly to soothe dryness.
- Lubricate: A water-based lubricant such as YES Water-Based Lubricant can make intercourse more comfortable by reducing friction. I also recommend considering oil based and silicone based lubricants to see which type is most comfortable for you. Have a read of our blog ‘Your Ultimate Guide to Lubricants: Comfort, Pleasure, and Health' for more information.
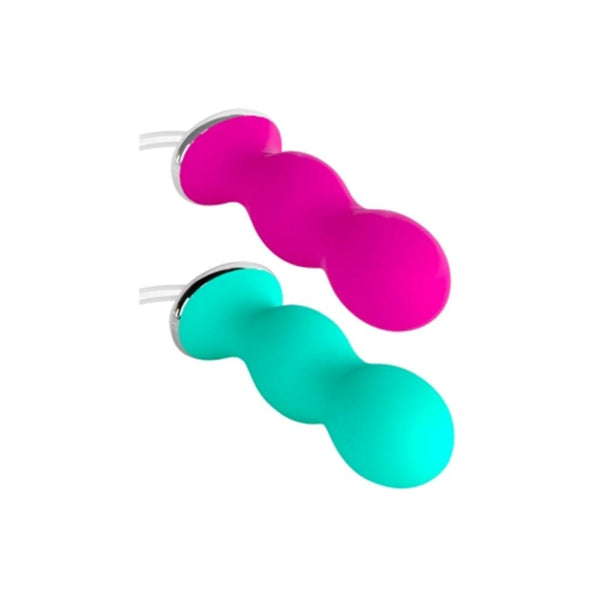
- Stay active: Regular sexual activity, including arousal and orgasm, helps maintain blood flow to the pelvic tissues, keeping them healthier and more resilient. There is some promising research coming out on the benefits of vibrators during menopause. We recommend vibrators made of medical grade silicone such as – The Swan Wand and The Swan Mini Wand.
- Maintain vaginal integrity: If you’re experiencing symptoms of vaginal atrophy (the thinning, drying, and inflammation of the vaginal walls due to a drop in estrogen levels), such as pain during intercourse, vaginal tightness, or dryness, dilators can be a helpful non-invasive solution. Dilators help by gently stretching the vaginal tissues, making them more flexible and improving comfort during sex or medical exams. You can view our range of vaginal dilators here.
- Consider hormone therapy: Talk to your doctor about using a topical hormone replacement therapy. More information about Low Dose Vaginal Estrogen Therapy can be found here.
Managing Urinary Incontinence During Menopause
Incontinence is a common concern during menopause due to weakening pelvic floor muscles. If you’re struggling with this, here are some helpful tips to manage it:
- Fluid timing: Sip your fluid throughout the day and avoid drinking fluids three hours before bed to reduce night time bathroom trips.
- Limit bladder irritants: Caffeine, alcohol, and spicy foods can aggravate incontinence. Reducing or eliminating these can help.
- Do pelvic floor exercises: Kegels and other pelvic floor exercises can help strengthen the muscles that control urination.
The Importance of Pelvic Floor Physiotherapy
Pelvic floor therapy can be incredibly beneficial during menopause. A pelvic health physiotherapist can help you manage symptoms like incontinence, pain during sex, and pelvic organ prolapse. They can also work with you to improve the elasticity of your vaginal tissues, preventing discomfort and promoting better bladder control.
Final Thoughts
It’s never too late to start thinking about your pelvic health. Whether you’re already experiencing menopause symptoms or are in the early stages of perimenopause, working with a pelvic floor physio can help you maintain strength and function, improving your overall quality of life.